Experience with the healthcare system for caregivers of dementia patients
In brief
Dementia patients are typically elderly and have several chronic diseases, demanding multiple healthcare visits yearly. Most live in the community and are assisted by unpaid family carers who frequently help with healthcare management. However, little is known about how caregivers and people with dementia interact with the healthcare system, which may be more challenging in the presence of cognitive disorders like memory loss.
Introduction
More than 16 million Americans provide daily help to people with dementia (PWD). Caring for people with disabilities differs from being a family caregiver for several reasons. First, as their physical, cognitive, and emotional abilities deteriorate, PWD requires more caregiver monitoring, dementia support with instrumental activities such as money management or driving, and self-care duties like washing and clothing. Second, PWD behavioural changes and communication challenges may increase caregiving demands and caregiver stress in later phases, leading to losses in caregivers’ mental and physical health.
PWD frequently deal with various chronic diseases and age-related changes, such as diminishing vision and hearing, because age is a critical risk factor for dementia patients. Therefore, a multidisciplinary team must provide continuous, comprehensive, and coordinated treatment for this complex network of functional impairments. Given PWDs’ increasing difficulties with memory and understanding, carers are critical advocates for PWD healthcare to help people with dementia inside and outside clinic visits. The limited data elucidates the actions that carers conduct related to PWD healthcare management, such as arranging visits, transporting PWD to appointments, giving history to clinicians, and executing care team recommendations. PWD, for example, may forget to take medicine or make home safety improvements, putting caregivers in charge.
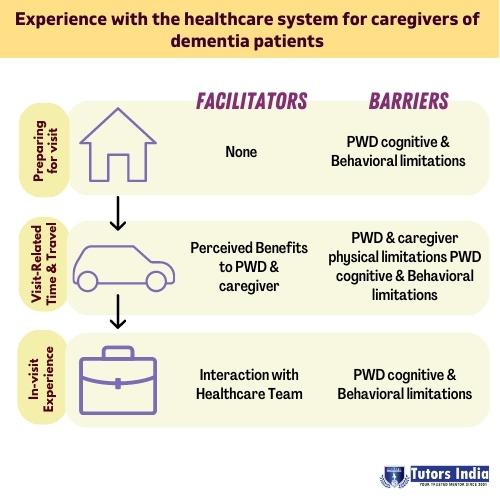
Three categories related to the experience of the healthcare system were identified: Preparing for a visit, PWD cognitive and behavioural limitations, Visit-related time and travel, PWD and caregiver physical limitations, Perceived benefits to PWD and caregivers
Preparing for visit
The process of mentally and emotionally preparing PWD for a medical appointment is referred to as “preparing for the visit.” The restrictions reported in this group’s caregiver responses were classified as PWD cognitive and behavioural impairments. There was no recognized sub-category for facilitators. The caregivers’ explanations of perceived difficulties are included below, along with, when applicable, facilitation techniques for removing obstacles and caring for people with dementia.
PWD cognitive and behavioural limitations
Physically getting PWD ready (such as bathing and clothing) was often difficult, according to caregivers. The procedure was described as “a tremendous production” and “a lot.” The approach was complicated by PWD’s old age and comorbidities, necessitating alterations to the morning schedule on the day of the visit.
Visit-related time and travel
The caregiver’s and the PWD’s travel arrangements, journeys to and from the visit, and experiences at the healthcare institution are referred to as visit-related time and travel.
PWD and caregiver physical limitations
For PWD and carers, physical limitations and declining mobility were obstacles to visit-related time and travel. The difficulty comes from thesis writing help attempting to get the PWD inside the offices, according to caregivers who recounted helping him with wheelchairs and walkers. This occasionally happened due to PWD weariness, which made travelling even short distances challenging.
Perceived benefits to PWD and caregivers
On the positive side, several caregivers found that attending medical appointments allowed them to socialize. Attending a visit was “an outing, and maybe we’d stop for lunch on the way home” because dyads “don’t go out much at all.” Some PWD considered the journey to the visit to be “pleasant because we got to drive through his old house.” A caregiver remarked that his father “chit-chats” with whoever is sitting on the bench and that he enjoys observing his father “happy and being healthy” due to this interaction.
Conclusion
The need for dementia-capable care that considers the complexity of the condition for patients with dementia (PWD) and their carers is expanding. From the perspective of family caregivers of PWD, this study highlighted three elements of interacting with the healthcare system, both during and after the visit, outlining possible barriers and facilitators. Despite obstacles brought on by PWDs’ physical and cognitive limitations, research findings point to viable care-optimization solutions. For example, attending medical appointments has additional benefits. The report also brings up issues with payment and their effects on family-centred dementia treatment.
Additionally, we assist you with writing dissertations, proposals, manuscript editing and writing, data collection, research methodology, cross-sectional studies, retrospective studies, case studies, critical reviews, and literature reviews. Masters dissertations help you with statistical analysis using regression while considering confounding effects, developing cutoffs, and General Linear Models (GLM), among many other computations, results, discussions, and recommendations.
References:
- Gately, Megan E., et al. “Experience of the healthcare system for caregivers of persons with dementia.” Aging and Health Research1 (2022): 100061.
- Piersol, Catherine Verrier, et al. “Effectiveness of interventions for caregivers of people with Alzheimer’s disease and related major neurocognitive disorders: A systematic review.” The American Journal of Occupational Therapy5 (2017): 7105180020p1-7105180020p10.

 Previous Post
Previous Post Next Post
Next Post