A Statistical Analysis on the Effectiveness of Cessation Programmes on Alcoholism
Tagged: Business and Management
Introduction
Alcohol is a widely used “addictive” substance. It can trigger a wide range of behavioural consequences as a psychoactive substance, including gregariousness, aggression, loss of control, and cognitive impairments. Although Alcohol Use Disorders (AUD) are diagnosed based on a wide range of reported symptoms, they are frequently treated as a binary outcome (unaffected or affected). Alcoholism, like all complex diseases, can be considered a clinical result caused by an interaction of multiple risk factors, and the alcohol-dependent population includes a number of individuals with varying sets of symptoms and disease severity (Lisa M. Hines, 2022).
AUD may be associated with concurrent psychiatric disorders (e.g., drug use disorders, major depressive and bipolar I disorders, certain phobias, and antisocial and borderline personality disorders) as well as somatic and psychosocial problems (e.g., liver disease; pancreatitis; malignancies of the neck, head, liver, colon, and rectum; accidental injuries, aggression, violence, and suicide). Alcohol is responsible for 5.9% of fatalities worldwide (7.6% in males and 4.0% in women), with cardiovascular disease and diabetes (33.4%), injuries (17.1%), gastrointestinal illnesses (16.2%), and malignancies (12.5%) being the primary causes (Kranzler HR, 2018).
In the UK, deaths from alcohol-related causes have increased from 11.8 per 100,000 in 2019 to 14.0 in 2020, witnessing a steep rise of 18.6%, being the highest rate of increase in over 20 years. According to the Office of National Statistics (ONS), alcohol-specific deaths or those directly associated with alcohol abuse were classified into three causes- alcohol related liver diseases (77.8% of deaths), mental or behavioural disorders resulting from alcohol (12.1%) and external causes, which include intentional or accidental poisoning or exposure to alcohol (6.2%). However, there may be an underreporting of the deaths.
Alcohol use disorder is frequently misdiagnosed and undertreated, and the management of alcohol-related liver disease caused by excessive alcohol consumption is difficult. Patients who have alcohol use disorder and alcohol-related liver disease need multidisciplinary care involving multiple specialists and therapeutic approaches, which can create barriers to successful treatment. Stigma, challenges in modifying health behaviours, a lack of understanding of the dangers of alcohol, and fragmented treatment are just a few of the issues that can make managing alcohol-related liver disease challenging. Integrated care is one step towards overcoming these obstacles; much might be gained from programmes for liver transplantation in patients with severe cirrhosis who have received successful multidisciplinary care (The Lancet, 2022).
There is currently no universally accepted definition of “recovery” in the field of alcohol treatment literature. There are several formal definitions of recovery from substance use disorders. Although these definitions differ, they all agree that recovery is an ongoing process characterised by improvements in functioning and well-being and that abstinence from alcohol or other drugs is an essential component. There are various modalities for treating alcoholism, starting with detoxification, aversion therapy and counselling (Hagman, 2022). Organisations like Alcoholics Anonymous, Al-Anon Family Groups, We Are With You and Adfam are beneficial in motivating and encouraging individuals to abstain from alcohol.
The study is aimed at understanding the effectiveness of alcohol cessation programmes on reduction in alcohol consumption alcoholism in Yorkshire. The paper originally hypothesises that significant differences in alcohol consumption will exist between the experimental and control groups following the intervention. The null hypothesis implies that there will be no significant difference in the intervention of cessation programmes on alcoholism.
Methodology
The study comprises 70 participants, with about 45 (64%) being male and 25 (36%) being female, aged between 20 to 75 years old. All the participants were diagnosed with alcoholism when they were shown to the General Practitioner. All participants underwent a detoxification session and took medications for alcohol aversion. The participants were categorised into experimental and control groups, with 35 participants being in each group.
The control group received a placebo. On the other hand, participants in the experimental group attended four cessation programmes, which comprised of testimonies and counselling sessions once per week. To protect the participants’ identities, they were assigned a code starting from A001.
Data was collected from the participants relating to the type, frequency (number of days of consuming alcohol and drinks consumed per drinking day (DDD) and quantity of alcohol consumed for the past 28 days.
According to the National Institute of Health Care and Excellence, DDD can be classified as:
- Abstinent (zero drinks for the past 28 days),
- Low to high (1-15 DDD),
- High to extreme (16-30 DDD), and
- Extreme (>30 DDD) (Eastwood B, 2018)
All the patients who were in sound mind were selected for the study. SPSS was used for analysing the data regarding the study participants and to assess the impact of cessation sessions on alcoholism.
Results
The study comprised of 70 subjects aged 34.3 years, with a standard deviation of 10.7 years. The participants have been drinking alcohol for 1 to 50 years (10.57 years ± 12.36 years). All the participants were from Yorkshire, UK. Based on DDD, the participants were classified as low to high (23.67%), High to extreme (45.72%). The remaining participants (30.31%) fall under the category of extreme.
Shapiro-Wilk test was used to determine the normality of the distribution of the participants. Since most of the participants have high to extreme and extreme DDD, a step-by-step approach to reduce alcohol consumption was implemented. The analysis revealed that the pre-intervention DDD, that is, N(70)= 13.25, p<0.005, and the post-intervention DDD, N(70)=10, p<0.005 were not normally distributed. Therefore, non-parametric tests like the Kruskal-Wallis and ANOVA were used.
Following the intervention, a significant difference between the treatments and the DDD was observed, with the placebo group increasing slightly to a mean of 18 DDD and the cessation group decreasing to 10. This shows that the intervention was effective in lowering the subjects’ alcohol consumption. Based on these observations, the null hypothesis is rejected and the alternative hypothesis is accepted.
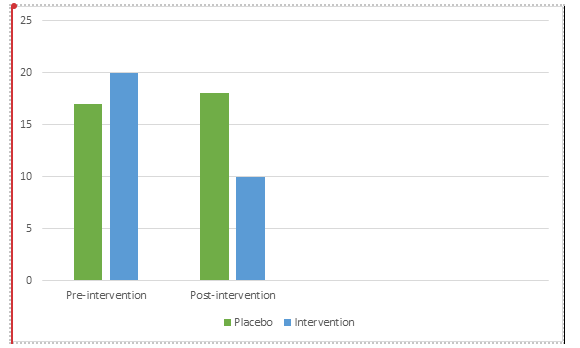
Figure 1: Mean showing the differences in the DDD between the categories before and after intervention
Discussion
The study examined the impact of four alcohol cessation programmes on lowering DDD and promoting and maintaining sobriety. The findings show that alcohol cessation programmes were beneficial for the population. There was a significant reduction in the DDD of those who attended the alcohol cessation programmes. The mechanism can be attributed to the motivation of individuals when they hear others’ testimonies.
The primary objective of the research was to determine whether or not the intervention had a positive effect. The findings demonstrate that the reduction in DDD was statistically significant. As a result, the study accepts the alternative hypothesis while rejecting the null hypothesis.
Conclusion
The study concludes that alcohol cessation programmes are effective in reducing the frequency and amount of alcohol consumed and can promote and maintain sobriety. Since AUD is a chronic condition, continued provision of support may encourage adopting healthier habits and prevent relapse. To know more about how statistical analysis is done in other subject domains, check out our data analysis examples.
References
- Lisa M. Hines, Lara Ray, Kent Hutchison & Boris Tabakoff (2022) Alcoholism: the dissection for endophenotypes, Dialogues in Clinical Neuroscience, 7:2, 153-163The
- Kranzler HR, Soyka M. Diagnosis and Pharmacotherapy of Alcohol Use Disorder: A Review. JAMA. 2018 Aug 28;320(8):815-824.
- Hepatology, T. L. G. (2022). Digging deeper into alcohol-related deaths. The Lancet. Gastroenterology & hepatology, 7(2), 107.
- Hagman, B. T., Falk, D., Litten, R., & Koob, G. F. (2022). Defining recovery from alcohol use disorder: development of an NIAAA research definition. American Journal of Psychiatry, 179(11), 807-813.
- Eastwood B, Peacock A, Millar T, Jones A, Knight J, Horgan P, Lowden T, Willey P, Marsden J. Effectiveness of inpatient withdrawal and residential rehabilitation interventions for alcohol use disorder: A national observational, cohort study in England. J Subst Abuse Treat. 2018 May;88:1-8.


